Hydration is a common phenomenon, affecting as many as 38% of drug molecules1.
There are plenty of hydrated drugs on the market, but how can an informed choice be made of which version to develop, the hydrate or the anhydrate?
Understand the system.
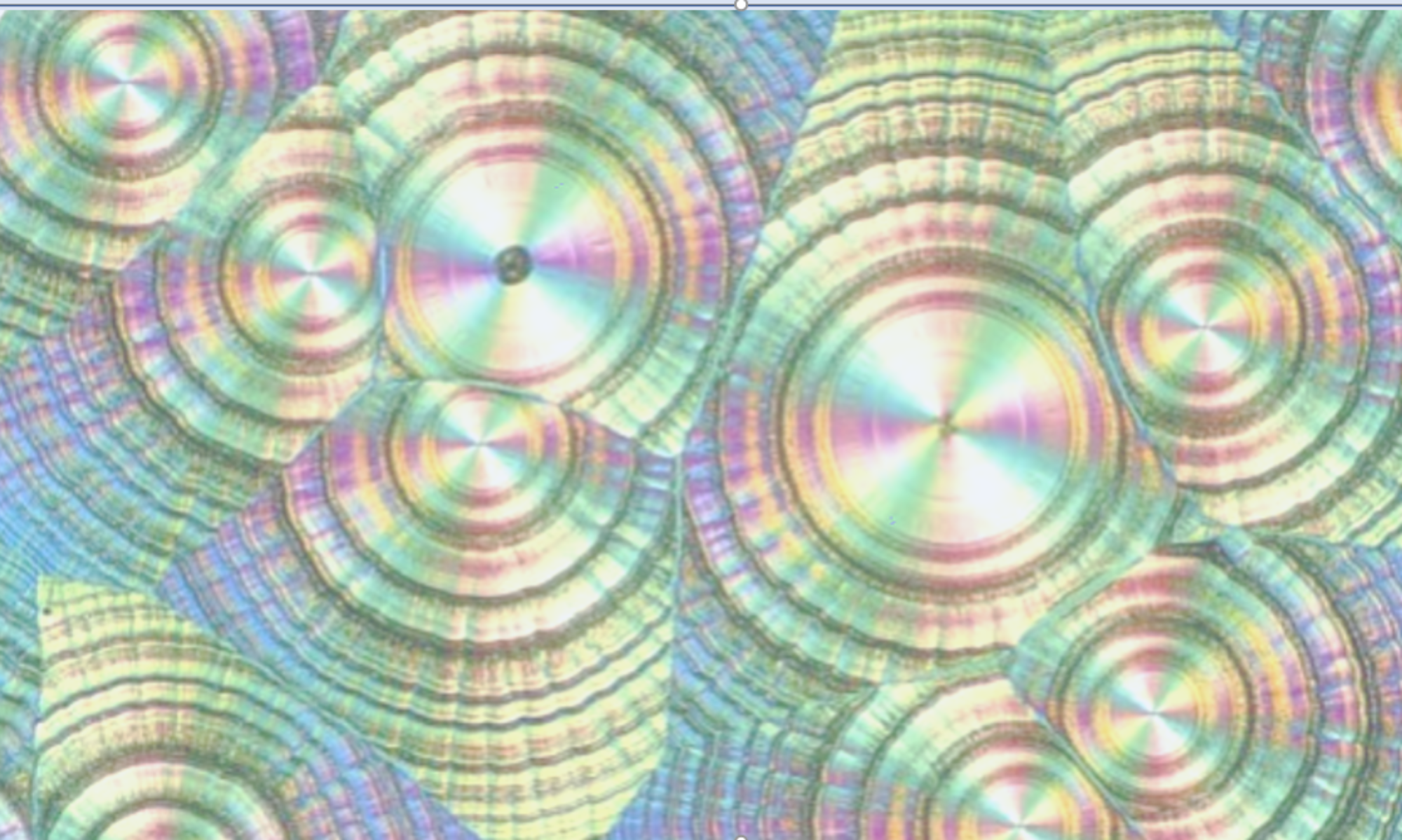
The first question to ask is ‘Do I have a hydrate?’ and as many polymorph screens do not specifically seek out hydrated versions, this may not be obvious. Aqueous/organic solvent mixtures should be incorporated into any polymorph screen that supports a version decision. If the polymorph screen doesn’t furnish new hydrated forms, then computational approaches such as the Cambridge Crystallographic Data Centre’s (CCDC) Hydrate Analyser can be used to assess the potential risk and might stimulate more in-depth experimental searches2. Conversion to a hydrate occurs once a critical water activity is reached. This is an important value and can be measured using dynamic vapour sorption (DVS) although as a kinetic measurement, DVS may not detect water uptake if it is slow 3. Better, is to slurry the API in aqueous/organic mixtures of known water activity and analyse the solid after equilibrating for a nominal period (DSC, TG, DVS, XRPD and of course KF) 4. Knowing the critical water activity is crucial in understanding the controls which might be required during manufacturing, storage and in-use, both for the API and the formulation. Also, Single Crystal X-ray Diffraction can provide an effective basis to rationalize the observed hydration/dehydration pathways. Hydrates in which the water is stable over a range of humidities and temperatures are much easier to develop than where hydration is partial, easily reversible, or where water is lost at typical conditions that might be encountered in a manufacturing plant.
How do the bioavailability, manufacturability and stability compare?
The hydrate normally has lower aqueous solubility than the anhydrate so might not be selected based purely on this criterion5. However, if the solubility absorbable dose can be achieved, then the hydrate should still be a potential candidate for development. This presents an interesting question. Should the hydrate be developed in preference to the anhydrate as dehydration will lead to higher not lower solubility? The solubility though isn’t the only consideration in formulation performance. Hydration during tablet disintegration can negatively impact dissolution rate and this might disfavour selection of the anhydrate as the developable version. This is seen in the case of Theophylline where the growth of an extreme hydrate habit impedes tablet dissolution6. Establishing potency of the formulation should also be considered, particularly where water gain and loss is facile; how much of the drug needs to be weighed-out when the formulation is manufactured? The other typical physical properties that make an API well behaved such as habit, powder flow, compressibility etc. should also be assessed as part of the decision7. Finally, the chemical stability of the anhydrate and hydrate may differ.
Will I have to control the hydration state in manufacturing, storage and in-use?
The need for control is also an important consideration in deciding between a hydrate and anhydrate. Humidity and temperature controls can introduce considerable complexity. In the API plant, the crystallisation, isolation and drying of the API might require a discrete step to achieve the desired solid state form and this might need to be maintained in bulk storage leading to a more complicated pack. Ambient humidity and temperature might require control during the manufacture of the formulation. More extreme conditions, for example less that 20% RH or more than 80% RH are difficult to achieve. Finally, in-use stability needs to be considered to ensure that the formulation is consistent with the label claim. All of this may require sophisticated and validated analytical methods to confirm the degree of hydration. For low dose compounds, particularly in the formulation, this presents a real challenge due to limits of detection.
To summarise, hydrate versions of drugs can be developed but the system needs to be understood and the impact of hydration state on the bioavailability, stability and manufacturability of the API and the formulation assessed. The final decision may be far from straightforward and may require trade-offs between optimum physical properties versus the control needed in manufacturing, storage and in-use.
References
- Estimates of how likely hydration is for molecular crystals vary. A survey of the Cambridge Structural Database showed 6.5% of structures were hydrated. See Motherwell http://dx.doi.org/10.1039/b612529. However, it must be assumed that not all structures are lodged in the database. The review from Stahly https://doi.org/10.1021/cg060838j uses polymorph screening statistics and is quoted here.
- For a review of Mercury 4.0 which includes the hydrate analyser, see https://dx.doi.org/10.1107%2FS1600576719014092
- See Edens and Newman in Polymorphism in the Pharmaceutical Industry p.235 ISBN 3-527-31146-7.
- For a comprehensive review of experimental techniques, see https://doi.org/10.1002/jps.21187
- See Higuchi https://doi.org/10.1002/jps.2600520815
- Hydrate formation for Theophylline can occur during wet massing if granulation is used in the formulation, or, at the point of tablet disintegration. https://doi.org/10.1016/0378-5173(92)90144-Q
- For an example of differences in tabletability directly ascribed to hydration, see the example of sodium naproxen. https://doi.org/10.1016/j.ijpharm.2010.01.036