Polymorphism, where molecules can pack in different ways in the crystal, is one of the most important considerations in drug development as different packing arrangements can exhibit different solubility in-vivo and hence impact safety and efficacy. Albendazole is a commonly used Anti-helminthic for the treatment of such conditions as cystic hydatid disease in both humans and animals. There are two main types of polymorphism; conformational polymorphism where the conformation of the individual molecules differs and this leads to different packing in the lattice, and packing polymorphism, where the molecular confirmation is the same, but individual molecules are packed differently in the lattice.

A B C
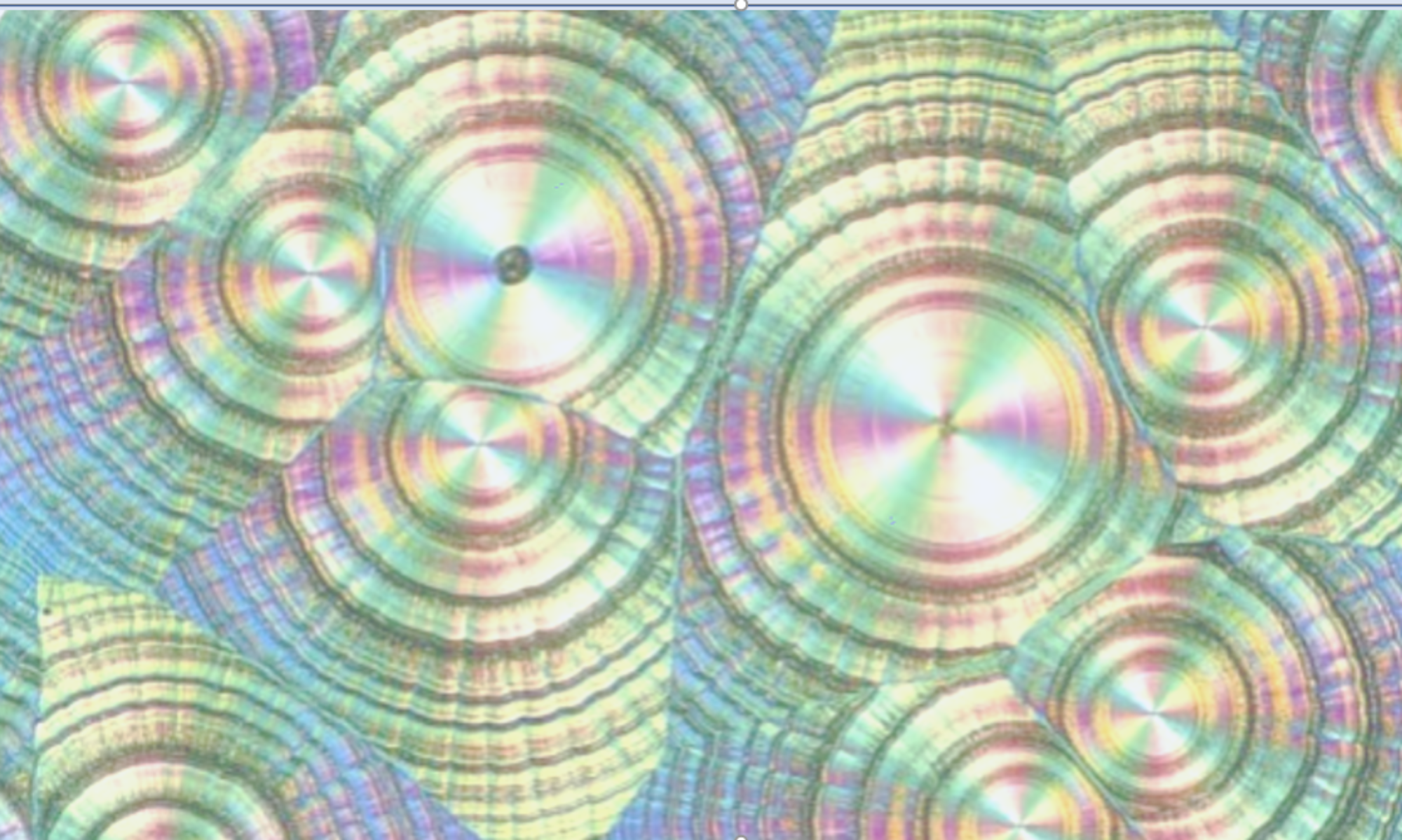
Figure 1. Structures A and B are related through packing polymorphism, whereas Structures A and C are related through conformational polymorphism.
Albendazole however, is a drug that falls into neither of these 2 categories. The commercial form of the drug is form 1. However, another polymorph, denoted form 2, also exists. The 2 polymorphs differ not merely through molecular confirmation or packing, but through proton transfer. In fact, the 2 forms are composed of molecules that are chemically different, Form 1 being the Amino form, and Form 2 being the Imino form, both forms being Tautomers of each other1. As they are chemically different, they are technically not even polymorphs! Unfortunately, there doesn’t seem to be a consensus on the descriptive term in the literature, and such examples of proton transfer can be described as ‘Desmotropes’ or as polymorphs. Figure 2 shows the chemical structure of the Tautomers. The picture is further complicated by disorder of the propylthio chain seen in the Xray crystal structure of Form 2; hence the representation in the structural formula in 2 positions on the Benzimidazole ring.

Figure 2. Tautomers of Albendazole. a. Amino Tautomer. B. Imino Tautomer showing disordered propylthio side chain (note, this is not disubstitution).
Delving into the literature more widely, polymorphs related through tautomerism are quite common. A further example is the anti-hypertensive Irbersartan2. In this case, the Forms are related to different protonation on the Tetrazole ring; Form A from the 1H tautomer and Form B from the 2H tautomer. As might be expected, there is a relationship between predominant tautomers in solution and the outcome of crystallisation from specific solvents. In a very elegant piece of work, using solvents of high relative permittivity and dipole moment, tends to lead to the crystallisation of Form B, whilst the reverse is true for Form A. The solvent favouring one tautomer over another in solution and hence leading to crystallisation of the specific form.
The whole area of polymorphs related through proton transfer, like Albendazole and Irbersartan, has been reviewed and the various scenarios classified in detail3. This paper shows the complexity encountered when proton transfer and tautomerism are overlayed with polymorphism.
References
- Enantiotropically Related Albendazole Polymorphs. Marco B. Pranzo, Dyanne Cruickshank, Massimo Coruzzi, Mino R. Caira, Ruggero Bettini. J Pharm Sci, 2010, 99 (9) 3731.
- The effect of solution environment and the electrostatic factor on the crystallisation of desmotropes of Irbesartan. Andrea M. Araya-Sibajaet al. RSC Adv, 2019, 9, 5244.
- A to Z of polymorphs related by proton transfer. Amy Woods-Ryan, Cheryl L. Doherty, Aurora J. Cruz-Cabeza. Cryst Eng Comm, 2023, 25, 2845.





Hi Alan – thanks for the questions. On the estimation of pHmax, Serajuddin (2007) provides examples of how pHmax is…